Diabetes/Prediabetes
MMC Simple Diabetes Treatment Algorithm
Clinical Goals
Ideal Blood Sugar Goals: Fasting Blood Sugars < 130. 2hr Postprandial Blood Sugars < 180. BP < 130/80 (Start with ACE or ARB and will likely need multiple medications). Urine Microalb 1x/yr. Statin for all patients > 40 y/o unless contraindicated. Yearly complete foot exam and eye exam. IF check chol, goals are LDL < 70-100, HDL > 40, TG < 200. Baseline EKG. Aspirin if CAD/Stroke. Healthy Eating, Regular Exercise (30 min/day+), Sustainable Weight Loss 5-7%. Ask about CV symptoms, and check weight, feet/peripheral pulses every visit. Quit Smoking!
Step 1 for all patients for glycemic control
Section titled “Step 1 for all patients for glycemic control”Step 2 if not at glycemic goals when recheck blood sugars or HbA1c
Section titled “Step 2 if not at glycemic goals when recheck blood sugars or HbA1c”ADD Sulfonylurea but beware hypoglycemia and long term metabolic consequences (weight gain, lipids, beta cell function).
AND/OR
ADD Pioglitazone (Actos) unless contraindicated (CHF) and titrate to max 45mg QD. Consider Spironolactone unless contraindicated to avoid/treat edema (25mgQD)
Step 3 if not at glycemic goals when recheck blood sugars or HbA1c
Section titled “Step 3 if not at glycemic goals when recheck blood sugars or HbA1c”Step 4 if not at glycemic goals when recheck blood sugars or HbA1c
Section titled “Step 4 if not at glycemic goals when recheck blood sugars or HbA1c”ADD short acting insulin with meal(s) by following 2hr postprandial blood sugars and titrating to 2hr postprandial blood sugar < 180 and HbA1c <7 (Stop Sulfonylurea).
OR
Change to Insulin Mix 70/30 BID or TID and titrate as above
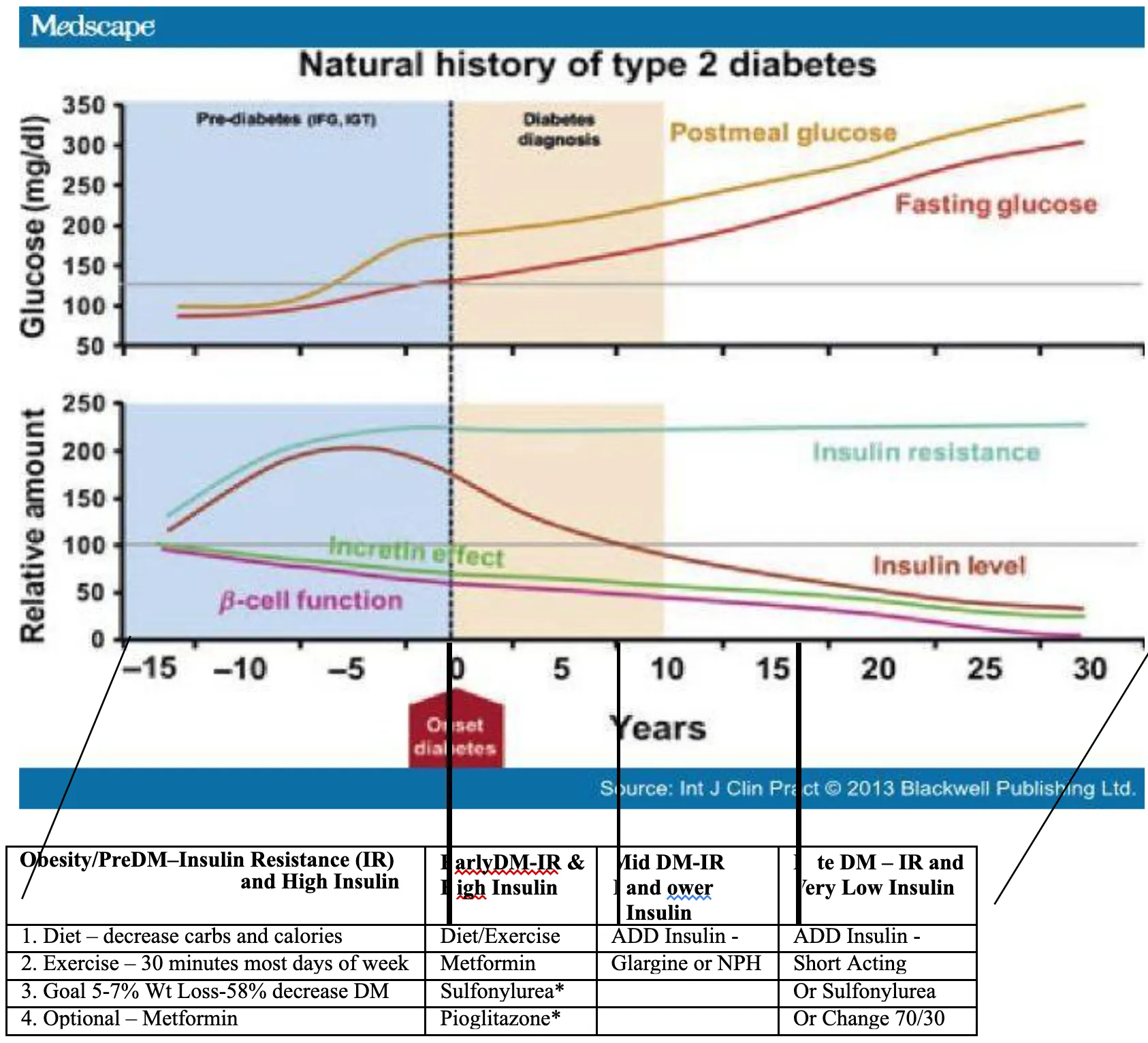 *Sulfonylureas can cause severe hypoglycemia. Sulfonylureas and Pioglitazone can cause weight gain and increased cholesterol.
*Sulfonylureas can cause severe hypoglycemia. Sulfonylureas and Pioglitazone can cause weight gain and increased cholesterol.
-
Background/Cultural Points:
Section titled “Background/Cultural Points:”Diabetes is an increasingly common disease in Cambodia, due primarily to genetic predisposition, low birth weights, and the high non-whole-grain (white) rice diet. Alcohol intake and obesity also contribute. Diabetes often presents classically (Polyuria, etc), but often presents at MMC as a patient’s-presumed-diagnosis based on a “high” random blood glucose test at a rural lab.
-
Work-Up/Diagnosis & Lab:
Section titled “Work-Up/Diagnosis & Lab:”- Make the diagnosis according to WHO criteria (HbA1c >= 6.5, FPG >/= 126 mg/dL or 7.00 mmol/L; 2h-PPG >/= 200 mg/dL or 11.10 mmol/L)
- Other labs: U/A is important to detect evidence of renal damage; ALT and Creatinine may be ordered to help determine best medication option and as baseline (Private lab acceptable)
- If fatigue is the presenting complaint, consider Hematocrit (in-house) and TSH (Pasteur Institute only) evaluations, etc.
- Consider: EKG if co-morbidities
-
Management/Education/Treatment:
Section titled “Management/Education/Treatment:”-
Patient Education:
- Explain the disease and its chronicity (incurable) to the patient.
- Teach the patient about the goal of treatment, prevention of complications
- Review Lifestyle Modifications: Weight Loss, Diet (Decrease Fat/Alcohol intake, decrease calories including decrease of white rice intake/substitute for brown rice); Increase physical activity. Diet – explain to patients that they may and should eat foods from ALL food groups, including fruits (Many Cambodians think DM2 management requires avoidance of fruits).
- Give patient DM2 Patient Information single page handout
-
Glucose Management Medications:
- If not contraindicated, Metformin is first-line (start low-dose to reduce nausea, and warn patient of initial SE)(Max: 500mg-850mg BID). Unless patient is clinically suspicious for Renal or Liver Failure, begin empiric treatment and order Creatinine as baseline (to review at follow up)
- Sulfonylureas (EG, glipizide) or Thiazolidinediones (EG, Pioglitazone) are also available in Cambodia; the former is cheaper, but causes weight gain and typically is effective for only 5-10 years. The latter is costly; SE: fluid retention, hepatic disease
- Insulin: difficult to procure in Cambodia; use as needed if resources allow
- Goal: Per WHO, A1C <6.5% is target (eAG = 140 mg/dL); however, the risks of tight control in this population may outweigh the benefits – it may therefore be reasonable to have a goal of A1C <7.0% (eAG = 154 mg/dL) or higher.
-
Other interventions/goals:
- Smoking & Alcohol cessation
- Tight blood pressure control (<130/80); ACEI = first-line; otherwise, consider HCTZ or Atenolol/Propranolol.
- ACEI (Enalapril 5-10mg QD) if proteinuria on U/A; otherwise, especially for rural patients, defer start of ACEI (Rationale: unlikely to be sustained by rural Cambodians; difficulty to monitor Cr/K). Monitor Cr/K q6-12 mos.
- Aspirin (ASA) low dose (325mg ¼ tab) if CAD risks additional to DM2 (Rationale: many Cambodians do not tolerate aspirin’s GI SE well; no coated version available; therefore, reasonable to defer ASA unless CAD risks significant (including age>40))
- Visual Acuity check in-house and fundoscopy (dilated exam per HCP skill); referral to Optometry for dilated-eye exam near time of diagnosis (if not done in-house)
- Counsel regarding foot care (wash and check daily; wear good fitting shoes with socks if able to afford)
- Vaccinations – advise annual flu, Pneumococcus (Age >65); not available at MMC
- Counsel women of child-bearing age regarding pregnancy (offer OCP; Metformin = Cat B)
- Home Glucose Monitoring is available at some pharmacies, but usually cost- prohibitive; therefore, may advise patients to check FPG weekly or monthly at a local lab, and return to MMC right away if FPG >
-
Follow-Up:
- 1 month f/u after initial diagnosis is reasonable (3 months if RPG <250-300 and patient from remote location); goal is every 6-12 month follow up.
- “Tight glycemic control” is goal, but without close monitoring, MMC goal is “looser” to avoid hypoglycemia and ensure reasonably sustainable regimen. FPG goal is <130 mg/dL or <7.22 mmol/L; Do NOT use HgbA1C unless NEEDED for clarification.
- At every 6-12 month follow-up, consider: FPG, U/A, Fundoscopy, Skin/Foot exam, Cr/K if indicated.
-