Hepatitis B
MMC Hepatitis B Treatment Recommendations – See Chart for who to treat/Treatment Recommendations below chart
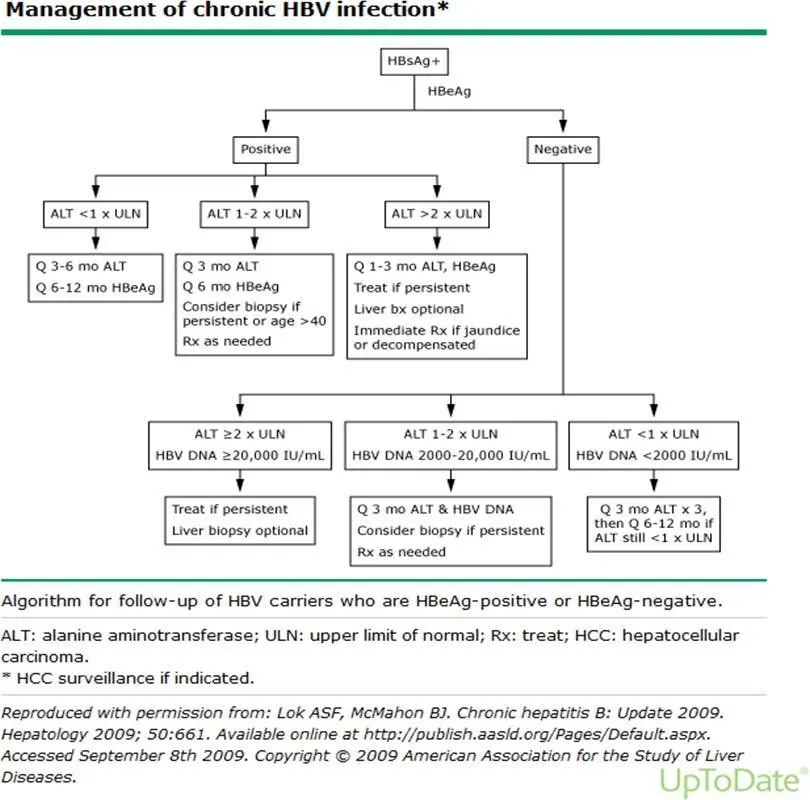
* For deciding whether to treat if ALT 1-2x normal, since liver biopsy isn’t available in Cambodia, estimate likelihood of fibrosis/cirrhosis by looking at ultrasound findings, other labs (PT, Albumin, Platelets) with risk scores such as FIB-4, and consider ordering Fibroscan at Calmette ($40).
Note – Consider using ALT for male <30 and female <20 as ULN – Upper Limits of “Normal”. To evaluate for fibrosis/cirrhosis, consider exam, ultrasound, and labs (platelets, PT, Albumin, etc.).
TREATMENT: If no past treatment, use Tenofovir if has resources and Lamivudine if poorer. Most patients require at least 4-5 years of treatment and indefinite treatment for many - especially if decompensated cirrhosis. If past treatment failure, use Tenofovir as resistance does NOT occur.
TENOFOVIR 300mg QD ($28/month? Now Cheaper?) (Note: Renally dose and monitor renal function Q3 months)
If initially Tenofovir and HBeAg+, continue one year PAST confirmed seroconversion to HBeAg- (second test at least 2 mo. later). Check HBeAg Qyr. Over the years, up to 50% of these patients will eventually have HBeAg conversion. After stopping meds, monitor for relapse/flare Q3-6months (ALT). Vload Q1yr?
If initially Tenofovir and HBeAg -, treat indefinitely (unless HBsAg converts (< 5%). Check Q1-2 years.
LAMIVUDINE 100mg QD ($3.75/month) If use Lamivudine, recheck viral load and ALT at 12 months. If ALT elevated and/or viral load detectable, switch to Tenofovir and then follow that protocol above. Otherwise, continue Lamivudine indefinitely. If initially HBeAg+, can stop 1 year PAST confirmed seroconversion to HBeAg- (2nd test 2+months later). If initially HBeAg -, continue indefinitely unless converts to HBsAg negative (5%). Check ALT Q3-6 months and viral load every year. If ALT elevates or viral load detectable, switch to Tenofovir and then follow protocol above.
Background and OLDER Protocol for Hepatitis B:
Section titled “Background and OLDER Protocol for Hepatitis B:”-
Hepatitis B infection is endemic in Cambodia due to vertical transmission. WHO’s EPI (Expanded Programme for Immunisation) has been implemented with much success since the late 1990s, reducing prevalence of Hep B, but there is no current program for adults to receive government-sponsored immunization. Around 25% of those infected develop cirrhosis/liver failure and/or Hepatocellular CA (HCC). Hep B is more destructive if acquired horizontally in adulthood. Management focuses on making a clear diagnosis, educating patients, preventing transmission, and preventing or delaying development of liver failure/HCC and preventing fulminant liver failure.
Background:
Section titled “Background:” -
Diagnosis:
Section titled “Diagnosis:”- If a patient has suspected Hepatitis B, this should be confirmed with a Hep B Surface Antigen (HBSAg) study (MMC Lab). Hep C Antibody screen (MMC Lab) is also recommended.
- If a patient needs general liver/GB evaluation, the following should be considered: Ultrasound, ALT/AST, CBC, albumin, PT/INR; Other chemistries (GGT, Alk Phos, Bilirubin studies) only if gallbladder disease suspected and results may change management;Consider HIV testing
-
Management/Education:.
Section titled “Management/Education:.”- Baseline ALT/AST (MMC Lab) should be ordered if not already done. If liver failure is suspected, Albumin (and possibly other liver function studies) should be ordered. If a patient has suspected liver failure, PT(INR)/PTT are unnecessary unless management of bleeding disorders is the goal.
- Liver Biopsy is NOT reasonable options in Cambodia for our patient population. Fibroscan is $40 at Calmette (2018).
- Tenofovir is drug of choice but more expensive. Lamivudine may be considered IF the ALT is >2-3X higher than normal upper limit. The patient should be advised that 70% of HBV will develop resistance to this single antiretroviral nucleoside analogue at 5 years and that the patient will need to cover the cost of the medication ($15usd/month). Lamivudine 150 mg per day can be used (usual dose is 100mg but 150mg is more cost effective in Cambodia).
- Ensure prevention of vertical transmission (HBIG + HB active immunization for newborns) and horizontal transmission (inform partner(s), use of condoms/abstinence).
- Provide protection:
- Educate the patient in avoidance of liver toxins. Abstain from alcohol. Do not use NSAIDs which can cause idiosyncratic liver toxicity. Paracetamol, in lower dose (<2g/day), is generally safe, and is dose-dependent.
- Advise Hep A vaccine (Pasteur Institute)
- See Background – explain cause and course/management goals of Chronic Hep B
-
Follow-Up:
Section titled “Follow-Up:”- It is reasonable to re-check ALT/AST only every 6-12 months